Our Solutions
The right data, the right way
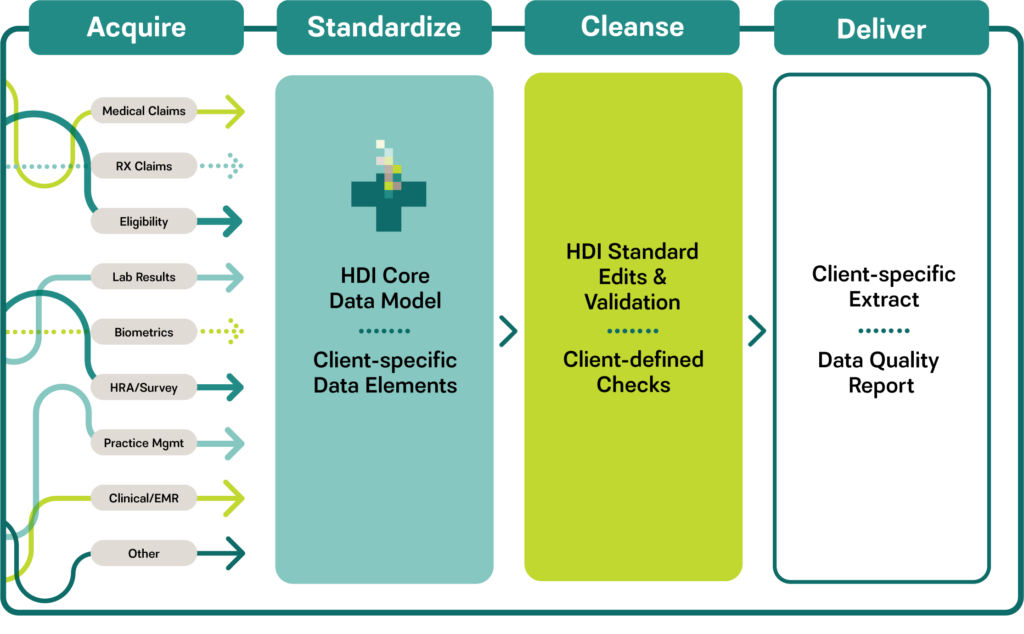
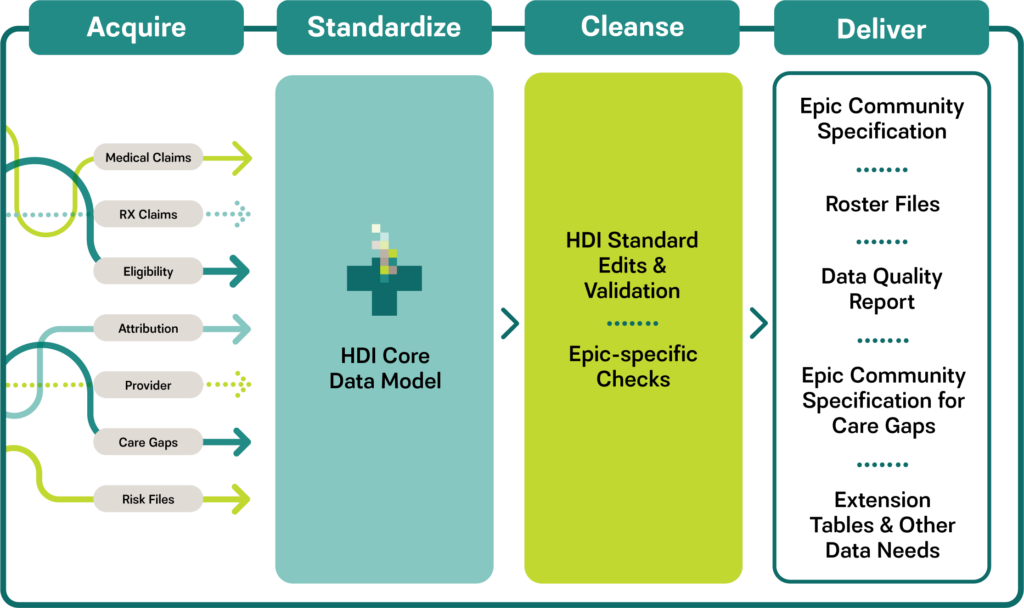
We help healthcare organizations integrate and manage data to support financial and clinical management, reporting, quality measurement, population health management, predictive/actuarial modeling, and other needs. We specialize in the acquisition, cleansing, and transformation of all types of health data including medical and Rx claims, eligibility and attribution, gaps in care, lab and biometric results, among others. We ensure data from disparate sources is mapped, standardized, cleansed, and delivered according to client-specific requirements and formats.
Contact UsData Standardization and Transformation
HDI helps clients acquire and integrate data from external sources into their data warehouse environment. Clients benefit from receiving data from multiple sources in a single, customized, easily consumable format that conforms to their data warehouse requirements.
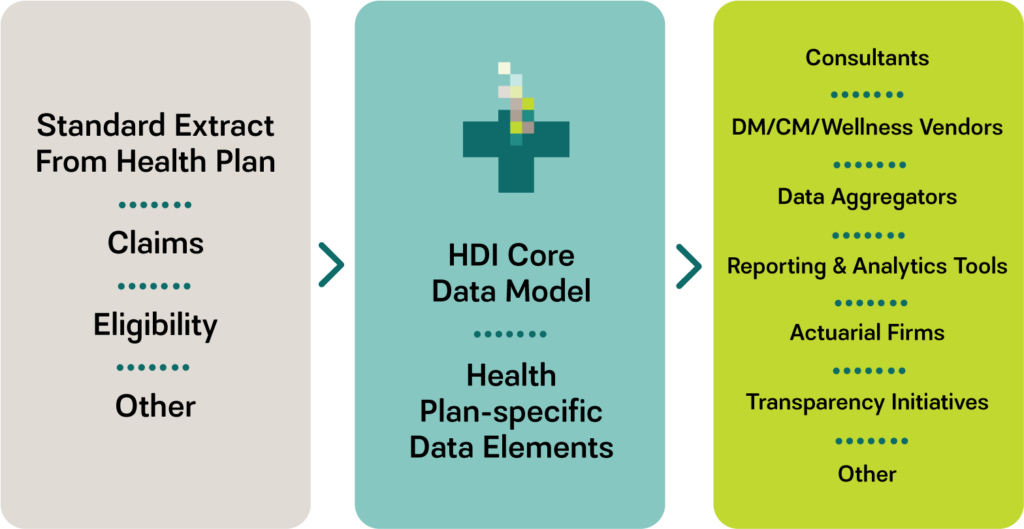
Health Plan Data Provisioning and Outbound Data Extract Creation
Supporting requests from vendors, consultants, and internal applications can be cumbersome and time consuming, particularly when a very specific layout is required. HDI can serve as the conduit for these requests, using our client’s standard extract as a starting point, and transforming and formatting the data to meet the content and layout requirements of each request.
Data Conversions
System conversions, rollout of new tools, and data warehouse changes can all drive the need for one-time projects to move data from one environment to another. HDI can support a health plan’s data conversion needs. In the process, data can be cleaned up, augmented, or aggregated to create a better, more efficient dataset.
Data Model Development
Not all of our clients have a data model robust enough to handle all of the types of data they want to access. HDI is happy to share our comprehensive, best of breed healthcare data model with our clients. We can also review and assess the suitability of an existing data model or data warehouse structure.

Member/Patient/Provider Matching and Data Augmentation
CMS and commercial carriers use identifiers that may not be meaningful outside their own organizations. HDI can match vendor-supplied data to our client’s own master member, patient, or provider files and append a client-specific identifier onto each claim. Sometimes clients want to augment either their internal data or externally-supplied data with information, for example, adding NPI numbers to a provider file or geocoding to a claims or eligibility file. HDI can identify reference datasets and append the new information during the data transformation process. Services can be provided on a one-time or ongoing basis.
DISCOVER THE HDI DIFFERENCE
Talk to our team today to learn how we can streamline your healthcare data integration and reduce the burden on your team.
Contact Us